Background - Thrombocytopenia and poor graft function(PGF) after allogeneic hematopoietic cell transplantation (HCT) may be defined as incomplete count recovery or late cytopenias not due to relapse. There is lack of evidence based treatment for PGF with commonly used modalities being supportive care, second transplants and CD34+ selected stem cell boosts. Eltrombopag, a thrombopoietin receptor agonist, stimulates proliferation and differentiation of hematopoietic stem cells (HSC). It has shown efficacy for PGF in observational studies, but is not approved for this indication. Cost of this drug is a major concern in state sponsored health care systems.
Methods - We retrospectively and prospectively collected data about patients who received Eltrombopag for thrombocytopenia and poor graft function after HCT. Post HCT thrombocytopenia was defined as persistent platelet count ≤ 20 x 10^9/l or transfusion dependence. PGF was defined if there was persistence of 2/3 cytopenias: thrombocytopenia, neutropenia (≤ 1.5 x 10^9/l) and/or haemoglobin ≤ 70g/l or transfusion dependence after day 28 of HSCT with complete donor chimerism and no evidence of relapse. Transplant characteristics, post-transplant complications and transfusion history was noted. In treated patients, Eltrombopag was initiated at 50 or 100mg daily and increased every 2 weeks to maximum of 150mg daily based on response. Response criteria: Complete Response (CR) - sustained platelet count ≥ 50 x 10^9/l, haemoglobin≥ 100g/L and ANC ≥ 1.5x10^9/L without transfusions; Partial response (PR) - platelet count 20-50 x 10^9/l or Hb 7-10g/L or ANC 0.5-1.5 x 10^9/l. Cost of transfusions were calculated from estimates of Canadian Blood Services and of hospital admissions were based on local hospital estimates. Cost estimation prior to Eltrombopag was calculated by the cost of supportive care from diagnosis of PGF or thrombocytopenia to initiation of Eltrombopag. Cost estimation post Eltrombopag was done by calculating the cost of drug intake + cost of supportive care (if any) after initiation of Eltrombopag. Primary outcomes were efficacy of drug and transfusion free survival; secondary outcomes were cost comparison between estimated cost prior to Eltrombopag and estimated cost after initiation of Eltrombopag.
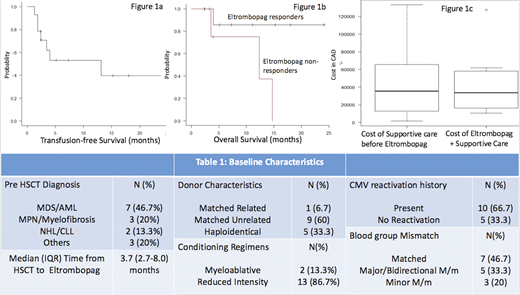
Results: 15 patients (males 66.67% (n=10); median age - 59 years) received Eltrombopag (Table 1). Indication of Eltrombopag was PGF in 86.7% (n=13) and isolated thrombocytopenia in 13.3% (n=2) patients. Response and cost analysis were limited to the 13 patients with at least 8 weeks follow-up after initiating Eltrombopag. After 8 weeks of Eltrombopag, Overall Response rate(ORR) was 76.9% (n=10; CR = 7; PR = 3). With median follow up of 6.2 months the drug was tapered or discontinued in 60% (n=6) patients showing response. All responders became transfusion independent within 8 weeks of maximum dose of Eltrombopag. The 3-month transfusion free survival after Eltrombopag was 70.7% (Figure 1A). Two out of three patients who did not respond to Eltrombopag died during the study period. The estimated median OS of non-responders vs responders = 12.4 months vs NR; p-0.063; Figure 1B). Eltrombopag was well tolerated with no incidence of serious adverse effects (Liver enzyme elevation, GI toxicity) to report. Rough estimates of cost analysis were done in patients who had response to Eltrombopag. These patients required median (IQR) of 15 (2-25) PRBC transfusions and 46 (32-96) pooled platelet transfusions with median 20 days of hospitalization due to cytopenia complications prior to 4 weeks after starting Eltrombopag. The median (IQR) duration of Eltrombopag exposure was 9.8 (6.3-25.6) weeks. The cost of supportive care before Eltrombopag was marginally higher than calculated total cost of Eltrombopag and subsequent supportive care treatment (Median cost 35311$ vs 33751 $CAD; p=0.9) (Figure 1C). The crude cost estimate of supportive care did not include cost estimates of human resources (including nursing), hospital visit time, time off work, and quality of life.
Conclusion - Eltrombopag is a safe and efficacious therapy for thrombocytopenia and poor graft function after allogeneic HCT with response in 77% of patients. Preliminary cost analysis shows that Eltrombopag is cost neutral by reducing supportive care and hospitalization costs and may be especially relevant in countries where supply of safe and adequate blood products is a challenge.
Lipton:Ariad: Consultancy, Research Funding; Takeda: Consultancy, Honoraria, Research Funding; Bristol-Myers Squibb: Honoraria; Novartis: Consultancy, Research Funding; BMS: Consultancy, Research Funding; Pfizer: Consultancy, Honoraria, Research Funding. Mattsson:ITB: Honoraria; Takeda: Membership on an entity's Board of Directors or advisory committees; Mallinkrodt: Honoraria; Jazz Pharmaceuticals: Honoraria; Gilead: Honoraria.
Eltrombopag is approved for ITP and Aplastic Anemia. It is currently not approved for thrombocyotpenia and poor graft function after Allogeneic Hematopoietic Cell Transplantation in Canada.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal